BCLC (Barcelona Clinic Liver Cancer) 2022 update
The BCLC classification, initially published in 1999, is regarded as the primary hepatocellular carcinoma (HCC) system by the American Association for the Study of Liver Disease (AASLD) and the European Association for the Study of the Liver. These endorsements, along with the significant contributions of hepatologists who developed the BCLC system, often overshadow the fact that not all clinicians and researchers in the field share the same viewpoint as these esteemed liver societies.
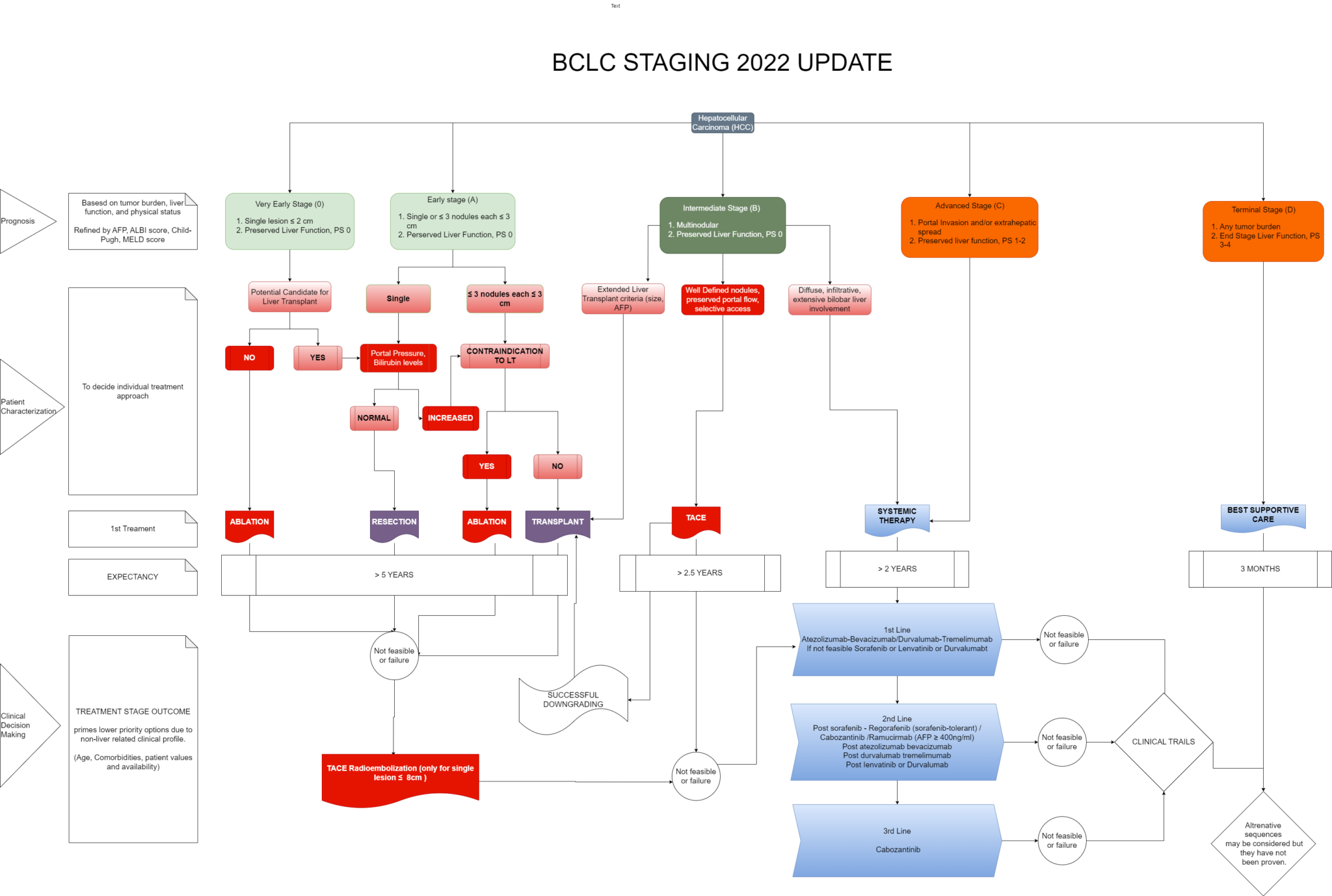
The BCLC system categorizes patients into five stages (0, A, B, C, and D) based on tumor stage, liver function, performance status, and overall well-being. This allows for a tailored approach to treatment, ensuring optimal outcomes. The BCLC treatment algorithm recommends different treatment options for each stage. Curative therapies like resection, transplantation, and ablation are preferred for early-stage HCC (stage 0 and A), while intermediate and advanced stages (B and C) may benefit from transarterial chemoembolization (TACE) or systemic therapies. Supportive care is recommended for patients with end-stage disease (stage D).
AFP and Radiological Assessment: The BCLC update emphasizes the importance of alpha-fetoprotein (AFP) and radiological evaluation in HCC diagnosis and staging. These tools aid in determining tumor burden, vascular invasion, and extrahepatic spread, facilitating accurate staging and treatment decisions.
Clinical Decision making:
- BCLC-0 Patients: For patients classified as BCLC-0, ablation techniques such as radiofrequency (RF) or microwave (MW) are the preferred treatment options.² ³ Percutaneous ethanol injection is still used in selected cases. If ablation is not feasible, surgical resection or transarterial chemoembolization (TACE) may be considered.4 Transarterial radioembolization (TARE) can also be effective for patients with single nodules ≤8 cm.5
- BCLC-A Patients: Resection and RF ablation offer similar survival benefits for HCC ≤2 cm.6,7 Ablation beyond this size is less effective, favoring resection instead. Microwave ablation (MW) is potentially the best option for patients with HCC ≤4 cm. 8,9 Larger tumors may still benefit from resection as long as there is no vascular invasion and sufficient remnant liver volume for adequate postoperative liver function.9,10 Radiation lobectomy through TARE may be considered in certain cases. Liver transplantation (LT) may be an option for patients with cirrhosis or specific tumor locations.
Treatment to Prevent Tumor Progression: In patients enlisted for LT with an expected waiting time exceeding 6 months, treatment options such as ablation, chemoembolization, and TARE can be considered to prevent tumor progression that may jeopardize LT.
Treatment for Multinodular HCC: The 2022 BCLC staging system does not recommend resection for multinodular HCC within Milan criteria. TACE is the preferred option if other treatments are not feasible. However, large tumors exceeding 8-10 cm and symptomatic patients (PS 1) may have worse outcomes after TACE.
Laparoscopic/Robotic Resection: Laparoscopic or robotic resection is a less invasive option with fewer postoperative complications. It may be considered in patients initially selected for ablation but with peripheral tumor location that contraindicates an ablative approach due to the risk of tract seeding or neighboring organ damage. However, it is important to consider the impact on liver function and the presence of portal hypertension. - BCLC-B Patients: Transarterial chemoembolization (TACE) is recommended if they have well-preserved liver function. However, increased bilirubin levels beyond 2 mg or slight fluid retention requiring diuretic treatment are associated with higher risks and suboptimal survival after TACE. Expert assessment is crucial in determining the appropriate treatment approach. TACE can be performed using conventional techniques, such as chemotherapy emulsified in lipiodol followed by embolic agent like gelfoam or PVA particles, or with drug-eluting microspheres (DEB-TACE). The response rates and survival outcomes are similar between the two techniques, so each team can choose their preferred method. Systemic treatment is recommended for BCLC-B patients who are not suitable candidates for TACE. If systemic treatment is not feasible, participation in clinical trials should be considered. Acceptable post-liver transplantation (LT) survival can be achieved in selected BCLC-B patients who do not meet the Milan criteria. Composite criteria considering surrogate markers of tumor biology, such as alpha-fetoprotein (AFP) levels and response to neoadjuvant treatments, may replace morphological criteria for defining transplant suitability. Downstaging approaches and careful patient selection may allow some patients to benefit from LT.
- For BCLC-C patients, first-line treatment options include atezolizumab-bevacizumab (Atezo-Bev) and the combination of tremelimumab and durvalumab. Tyrosine kinase inhibitors (TKIs) like sorafenib or lenvatinib can be considered when other options are contraindicated. Treatment decisions should be based on the patient’s clinical, radiological, and biochemical profile, aligned with the target population enrolled in clinical trials. Transarterial radioembolization (TARE) has shown promise in patients with liver-only involvement compared to sorafenib. However, prospective phase III trials comparing TARE to sorafenib or combination therapies have not demonstrated superiority or non-inferiority.
- BCLC strategy for prognosis prediction and treatment recommendation: The 2022 update
- Shiina S, Teratani T, Obi S, Sato S, Tateishi R, Fujishima T, Ishikawa T, Koike Y, Yoshida H, Kawabe T, Omata M. A randomized controlled trial of radiofrequency ablation with ethanol injection for small hepatocellular carcinoma. Gastroenterology. 2005 Jul 1;129(1):122-30.
- Germani G, Pleguezuelo M, Gurusamy K, Meyer T, Isgrò G, Burroughs AK. Clinical outcomes of radiofrequency ablation, percutaneous alcohol and acetic acid injection for hepatocelullar carcinoma: a meta-analysis. Journal of hepatology. 2010 Mar 1;52(3):380-8.
- Burrel M, Reig M, Forner A, Barrufet M, de Lope CR, Tremosini S, Ayuso C, Llovet JM, Real MI, Bruix J. Survival of patients with hepatocellular carcinoma treated by transarterial chemoembolisation (TACE) using Drug Eluting Beads. Implications for clinical practice and trial design. Journal of hepatology. 2012 Jun 1;56(6):1330-5.
- Salem R, Johnson GE, Kim E, Riaz A, Bishay V, Boucher E, Fowers K, Lewandowski R, Padia SA. Yttrium‐90 radioembolization for the treatment of solitary, unresectable HCC: the LEGACY study. Hepatology. 2021 Nov;74(5):2342-52.
- Cho YK, Kim JK, Kim WT, Chung JW. Hepatic resection versus radiofrequency ablation for very early stage hepatocellular carcinoma: a Markov model analysis. Hepatology. 2010 Apr;51(4):1284-90.
- Cucchetti A, Piscaglia F, Cescon M, Colecchia A, Ercolani G, Bolondi L, Pinna AD. Cost-effectiveness of hepatic resection versus percutaneous radiofrequency ablation for early hepatocellular carcinoma. Journal of hepatology. 2013 Aug 1;59(2):300-7.
- Yu J, Yu XL, Han ZY, Cheng ZG, Liu FY, Zhai HY, Mu MJ, Liu YM, Liang P. Percutaneous cooled-probe microwave versus radiofrequency ablation in early-stage hepatocellular carcinoma: a phase III randomised controlled trial. Gut. 2017 Jun 1;66(6):1172-3.
- Violi NV, Duran R, Guiu B, Cercueil JP, Aubé C, Digklia A, Pache I, Deltenre P, Knebel JF, Denys A. Efficacy of microwave ablation versus radiofrequency ablation for the treatment of hepatocellular carcinoma in patients with chronic liver disease: a randomised controlled phase 2 trial. The lancet Gastroenterology & hepatology. 2018 May 1;3(5):317-25.
- Chan AW, Zhong J, Berhane S, Toyoda H, Cucchetti A, Shi K, Tada T, Chong CC, Xiang BD, Li LQ, Lai PB. Development of pre and post-operative models to predict early recurrence of hepatocellular carcinoma after surgical resection. Journal of hepatology. 2018 Dec 1;69(6):1284-93.
- Raoul JL, Forner A, Bolondi L, Cheung TT, Kloeckner R, de Baere T. Updated use of TACE for hepatocellular carcinoma treatment: How and when to use it based on clinical evidence. Cancer treatment reviews. 2019 Jan 1;72:28-36.